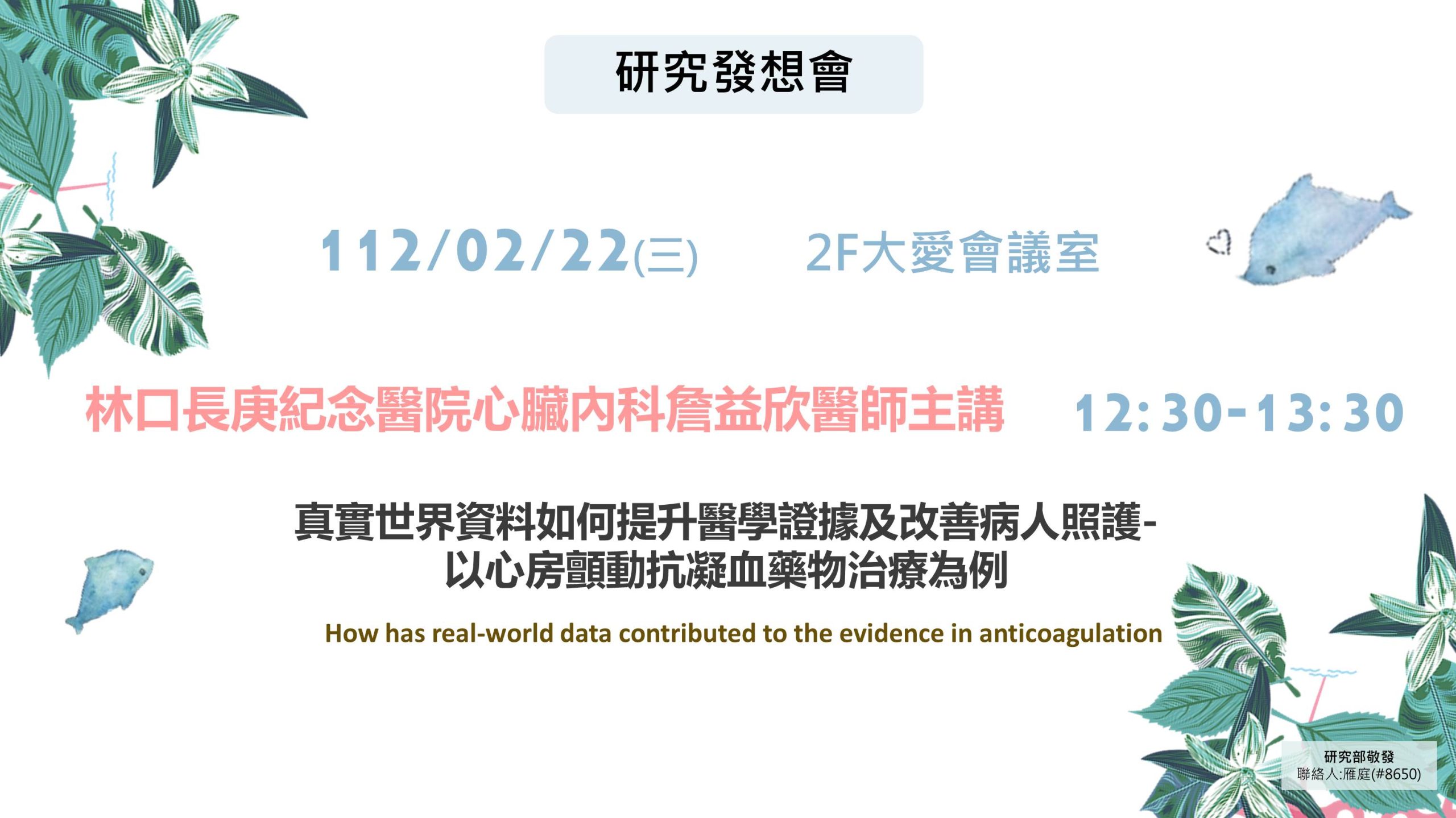
112年2月22日(三)12:30於2樓大愛會議室舉辦「研究發想會」,由林口長庚紀念醫院心臟內科詹益欣醫師主講「真實世界資料如何提升醫學證據及改善病人照護-以心房顫動抗凝血藥物治療為例」,歡迎有興趣的同仁前往聆聽。
本次講座摘要:
Real-world data confirmed the long-term consistency of effectiveness (ischemic stroke/systemic embolism: <1.91 per 100PYs) and safety (major bleeding: <1.61; Intracranial hemorrhage: <0.46; gastrointestinal bleeding: <1.06 per 100 PYs) of non-vitamin K antagonist oral anticoagulants (NOACs) in relative to warfarin in patients with non-valvular atrial fibrillation (NVAF) in Taiwan’s real-world practice. Previous studies indicated that Asian AF patients had a higher risk of intracranial hemorrhage compared to non-Asians treated with NOACs suggesting that Asians are more prone to bleeding. Therefore, clinicians in Asia tend to prescribe a lower dose of NOACs for their patients in the daily practice. However, our analysis indicated that an Off-label low-dose NOAC is not safer but harmful than on-label NOAC in risk of stroke in Asia’s real-world practice. Considering using the appropriate formula to determine each patient’s renal function and appropriate NOAC dosage, our study suggested using the CG formula rather than MDRD or EPI formula to estimate renal function and determine NOAC dosage in line with the guideline and RCT trials. Also, Real-world data confirmed the effectiveness and safety of NOACs in relative to warfarin in high-risk patients with NVAF (very elderly, ICH, advanced liver disease, thyroid disease, anemia, thrombocytopenia, cancer, or high atherosclerotic burden…) in Taiwan’s real-world practice. However, the real-world data indicated NOACs did not provide further benefit in effectiveness and safety over warfarin in NVAF patients with ESKD. We recommend individualized anticoagulation regimens after shared decision making with high-risk patients, based wherever possible on risk of stroke, bleeding, and patient values. Finally, we should watch out/Monitor the risk of kidney injury/GFR decline in AF patients with multiple risk during OAC treatment. The real-world data indicated that NOAC may be associated with a lower risk of acute kidney injury or a slower eGFR decline than warfarin in AF patients taking OAC. Furthermore, vigilance in monitoring for any potential adverse lung outcomes associated with the use of NOAC is recommended as part of the holistic approach to AF care and management.